
These oscillating moods can be so extreme and dramatic that it is a struggle to maintain a good quality of life, both personal and professional, which affects our all-around wellbeing. Moving between the two states is extremely destabilising, but each state in itself is an isolating and also potentially dangerous place to be.
Manic episodes are characterised by:
Although manic episodes encompass what would be considered ‘positive’ disposition, it can be exhausting, as there is no control or balance, and we are riding the extreme wave of our emotions. It can often feel like our brain is in overdrive going faster than us and we can’t keep up. These episodes usually last for a week or more and impact daily life severely, as normal day to day tasks are not the focus and we are distracted by our own wild and exuberant ideas.
After a manic episode, as we start to spiral downwards, we can often be left feeling drained after the high energy we expend. This is often accompanied by feelings of shame and anxiety regarding our behaviour as in the throes of the high, we may have over-committed to tasks which we are no longer in a position to pursue. In addition to this, we may find ourselves more isolated than before if we have ended or damaged relationships with the people closest to us who would not support our ideas during our manic state. This is one of the reasons why bipolar disorders affect not just individuals but family and friends too.
Depressive episodes are characterised by:
Depressive episodes can be particularly difficult to deal with after a period of mania, as the extreme high can make the low seem excessively low and we may often feel isolated from family and friends too. This is why having a trusted support plan in place is essential.
There are two other ‘mood’ episodes which individuals with bipolar disorder can encounter or experience - mixed episodes and psychotic symptoms.
Mixed episodes occur when you are experiencing both a manic and depressive episode simultaneously. These can be particularly difficult as there is no clear direction for the moods you are feeling. This can be overwhelming and tiring both mentally and physically. It may be harder to identify the support you need and for others to support you in the right way.
Not all individuals with bipolar disorder experience psychotic symptoms, but a few do, especially during the manic episodes. Delusions and hallucinations are common, seeing things that aren’t there or believing in things that are not real, which can lead to even more erratic behaviour.
Diagnosis for bipolar disorder is made by your doctor or GP after analysing your symptoms and mood over time, as well as some physical checks of other potential causes, such as your thyroid, which when out of kilter can provoke mania-like symptoms.
Once you’ve been diagnosed you may come up with a support plan with your doctor who often prescribes various medications to either to be taken daily to balance your mood or just for when you are experiencing a depressive or manic period. It’s thought that the best way to manage bipolar disorder is a mixture of complementary medicine, support and therapies. With the right plan, symptoms may only last around 3 months.
MD, FRCPsych, DPM, Msc, MBBS
Consultant Psychiatrist and CBT Specialist
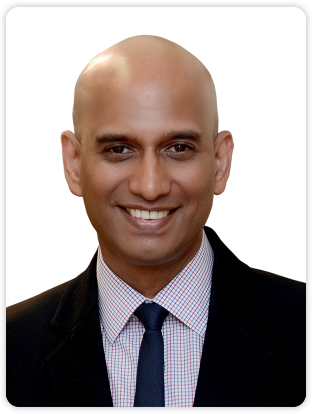

Dr Pereira helps patients to meaningfully understand, make peace, develop insight and let go of the past – to be precise, clear, connected, resourceful, calm and engaged with the present, in order to release mental space, energy and contentment for the future.
Established private practice
in the City of London
since 1993












